How Does Physical Therapy Help with Treating Lumbar Disc Herniations?
What is a lumbar disc herniation?
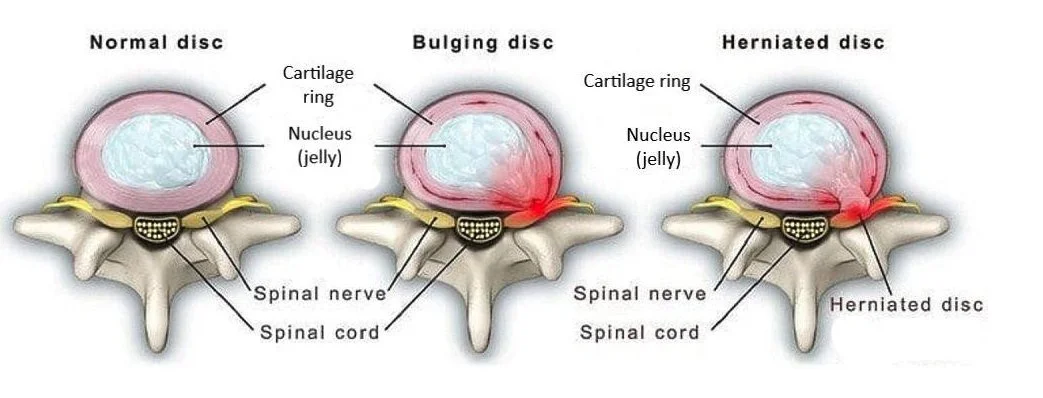
A lumbar disc herniation is when the inside part of the intervertebral disc (nucleus pulposis) extrudes through the outer rings of the disc (annulus fibrosis). Sometimes the term disc herniation and disc bulge are used interchangeably, but a disc bulge does not extrude through the annulus tissue.
Image from Neurosurgery One
A common term we hear is “slipped discs.” Please be aware that discs do not slip into and out of place. That is a common myth. Disc material is reabsorbed towards its original location over a period of months as the disc injury heals. How much of that disc material is reabsorbed varies, but (interestingly), this study found that the more massive the disc injury, the more healing occurred.
Common Lumbar Disc Herniation Causes
Lumbar disc herniations can be caused by many factors- we mostly commonly see them happen in one of two ways:
Acute onset: a sudden bending and/or twisting of the spine under load (when lifting something like a couch, heavy box, or deadlifting at the gym, etc.)
Longer term weakness, immobility, and poor posture/ergonomics
According to the research, lumbar disc degeneration is more prevalent in adults 50 years of age or younger with back pain compared with asymptomatic individuals.
Another study showed that progressive disc degeneration is seen with aging, and that in patients with low back pain, it is significantly accelerated.
However, this systematic review found that lumbar spine degeneration was present in high proportions of asymptomatic individuals (increasing with age). The key word here being ASYMPTOMATIC (these people had no pain at all, yet they had all kinds of “positive” findings on their imaging). The researchers suggest that many imaging-based degenerative features are likely part of normal aging and unassociated with pain. This is why we always perform a thorough clinical examination- to confirm whether or not the MRI findings are relevant to the patient experience. As the researchers state, “findings must be interpreted in the context of the patient's clinical condition.”
Lumbar Disc Herniation Symptoms
The most common symptoms associated with a lumbar disc herniation are low back pain with radiating pain that travels down the back of the leg/thigh, past the knee, and into the calf/foot. This is what some people refer to as the umbrella term of “sciatica.”
We often see these symptoms follow what we call a “dermatomal pattern.” This is when symptoms travel in an expected pattern down the back and into the leg.
Patients describe their symptoms as numbness, tingling, or burning. Symptoms are normally worse with sitting, getting up from sitting, trying to “straighten up” their spine, and with forward bending. Symptoms are usually best with stomach laying, standing, and walking.
Time of day strongly influences pain in patients who have a lumbar disc injury. Mornings are worse, and symptoms progressively get better as the day progresses. This is the case because the disc material rehydrates overnight (it absorbs more water). When you first get up and load the disc material (due to gravity), the sensory system is aggravated by the sudden loading and compression on the rehydrated intervertebral disc.
Diagnosing Lumbar Disc Herniations
A lumbar disc herniation can be ruled in or out with a battery of tests that we perform.
Straight leg raise (SLR) test: this is a sensitive test, which means that if the test is negative, we can be pretty confident that the patient doesn’t have a disc herniation. However, this test is not very specific, meaning that just because it’s a positive test, doesn’t mean we can confidently rule in a disc herniation. This is because there can be other reasons for why the nerve root that we’re stressing may be getting aggravated.
Slump Test: this is a very specific test, which means that if the test is positive, we can be really confident that the patient has a disc herniation.
Reflexes: if a patient has a disc herniation, we may see diminished reflexes at the level of the disc injury.
Weakness: if a patient has a disc injury, we may see weakness of the muscles that are getting nerve supply from the nerve root that comes out at the level of the spine where the disc injury is. This is more concerning, and will likely require medical interventions such as a corticosteroid injection or microdiscectomy surgery.
How Does Physical Therapy Treatment Relieve Lumbar Disc Herniation Pain?
Physical therapy treatment helps to relieve lumbar disc herniation pain by decreasing nerve sensitivity. We do this through a few different treatment techniques:
Modalities: ice/cold pack with transcutaneous neuromuscular stimulation (TENS)
Directional Preference-Based Movements: typically movements into extension are desirable to those with disc herniations. We find a tolerable entry point and increase the depth into extension, as tolerated.
Joint Mobilization: this helps provide the mechanical sensation that the disc material is returning to its original position (even though that isn’t actually occurring - time is what allows that reabsorption to happen). However, the sensation of that helps with symptom relief.
Soft Tissue Massage / Trigger Point Therapy: this helps to relax the tense muscles around the nerve root that are going into spasm to protect the nerve root.
How Long Do Herniated Discs Take to Heal?
Lumbar disc herniations typically take 8-12 weeks to heal. Timelines can be longer depending on the acuity of pain, and based on the individual's perception of what this injury means. We often see clients develop fear avoidant behavior as a result of their lumbar disc herniation, and that increases the likelihood of this developing into chronic/persistent pain. In other words, your mindset makes a difference in these circumstances.
There can be persistent sensitivity of the nerves in the surrounding area if muscles stay in spasm and/or if the nerve doesn’t regain its mobility (a concept we refer to as neural tension).
Things to Temporarily Avoid with a Herniated Lumbar Disc
In the early stages after a lumbar disc herniation, it makes sense to avoid provocative positions. Most commonly, those positions are prolonged sitting and forward bending.
With respect to training, we typically recommend avoiding high spinal loading activities such as deadlifts and squats. It’s recommended that you review different exercises and movement patterns with your physical therapist to determine which exercises you can and can’t handle based on your current circumstances.
Provided that walking doesn’t exacerbate your symptoms, we often encourage walking, to tolerance.
Best Exercises for Lumbar Disc Herniation
Some of the best exercises to use when rehabbing from a lumbar disc herniation include extension-based movements, side glides (especially if there is a hip shift present), and nerve flossing techniques.
Here are some extension based movements, in order of level of difficulty.
Cobras
Supermans
Back Extensions
Here are the side glides we typically use if someone has a hip shift. A word of caution that these are not easy to implement without the help of a trusted professional.
Side Glides
Left Lateral Shift
And here are some sciatic nerve mobility exercises we utilize when our patients are having radiating pain, in order of difficulty.
Going Back to the Gym After a Lumbar Disc Herniation
When going back to the gym after a lumbar disc herniation, it’s important to be reasonable about how you reload your system. This is especially important if you have fear or anxiety about getting back to squats and deadlifts. We coach our clients on a concept called “graded exposure”, talked about in this article. This is a concept in which we slowly reintroduce deeper ranges of motion and exercise volume as someone gets more comfortable and less fearful.
When making decisions about exercise, we don’t need pain-free to be the goal. We tell our clients that if you feel some pain or discomfort that dissipates fairly quickly, doesn’t exceed a 4/10, and returns to baseline within 24 hours, that’s perfectly okay. We don’t want to cause excess fear around feeling pain. Pain is just a signal to dial it back if the brain and body don’t like something. Listen to it, but don’t ruminate over it and consistently look for pain cues. If pain falls outside of the acceptable ranges discussed above, then you’ll need to dial back the intensity, frequency, and/or volume of your training.
If you’re interested in learning more about how to safely progress your deadlift after a low back injury, we outline that in a previous blog on deadlifting.
When to Consult a Medical Doctor or Surgeon
When working with our patients, we often refer to a medical doctor if the patient’s pain isn’t dissipating with conservative interventions. A medical doctor can recommend a prescription grade anti-inflammatory, oral corticosteroid, or a corticosteroid injection to reduce inflammation in the area and decrease pain. We find that patients with high pain levels, that aren’t decreasing with time and PT interventions, are able to participate in PT treatment much more comfortably once they utilize these medical treatments. These treatments provide us with a greater opportunity to facilitate mobility of your spine, and allow us to help you load the muscles without pain more easily.
If you’re experiencing worsening neurological symptoms such as numbness, tingling, muscle weakness, muscle atrophy, tripping over your foot when walking, or any bowel or bladder dysfunction, we recommend consulting with a medical doctor / surgeon as soon as possible. These can be emergent situations, and delaying care can result in long term nerve damage.
Closing Remarks
If you are experiencing lumbar disc-related pain and would like to consult us, please contact us below to speak with a physical therapist.
Disclaimer: This is not intended to be formal medical advice. Your individual needs should be met by the appropriate health care practitioner. Please consult with a trusted provider.
Dr. Paul Nasri, PT, DPT, OCS, COMT
Doctor of Physical Therapy
Orthopedic Clinical Specialist
Certified Orthopedic Manual Therapist