Shoulder Impingement Exercises
Physical Therapy for Shoulder Impingement
What is shoulder impingement / subacromial pain syndrome?
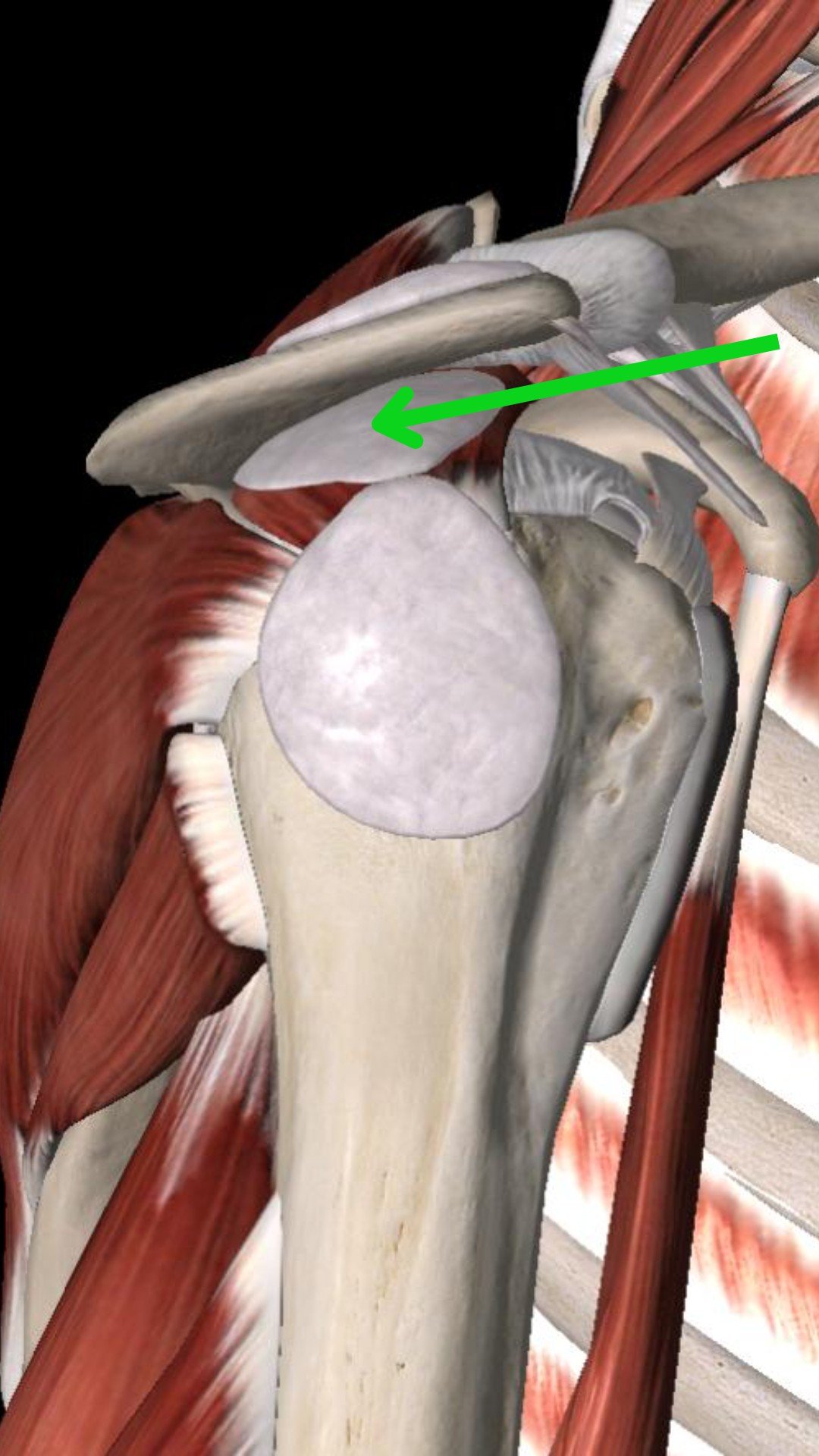
Shoulder impingement (now referred to as subacromial pain syndrome) is shoulder pain that occurs when soft tissue structures in your shoulder are compressed underneath the acromion. Your acromion is a part of your scapula (shoulder blade) (see image below).
Subacromial Space
Some of the structures in question are the rotator cuff (RTC) muscle, RTC tendon, and subacromial bursa.
There are 2 main types of this external shoulder impingement:
Primary Impingement (which is related to the shape of the acromion)
Secondary Impingement (which is related to decreased dynamic stability of the shoulder muscles, especially relevant with excessive overhead movement/lifting).
Acromion Types
Shoulder impingement symptoms
There are some common symptoms that are present when clients are dealing with shoulder impingement syndrome.
The most common symptom is pain in the subacromial and/or lateral (outside) part of the deltoid shoulder muscle. These symptoms are not usually present when the individual is at rest. Symptoms are worse when lifting the arm overhead.
Location of Shoulder Impingement Pain
Anterolateral Area
Deltoid Tuberosity Area
Posterior Area
The structures referenced earlier are most likely to be aggravated when lifting the arm out to the side of the body. Impingement symptoms are felt the most during something called the “painful arc.” The painful arc is at 60-120 degrees of shoulder elevation (abduction and/or flexion). Therefore, an individual will feel no pain when they begin to lift their arm overhead, then they will feel pain between 60-120 degrees. Once they lift above that point, the structures are no longer being compressed, so the client will say that they stop feeling pain.
Diagnosing shoulder impingement syndrome: Shoulder impingement vs. Rotator Cuff Tear, Frozen Shoulder vs. Shoulder Impingement
Shoulder impingement syndrome is diagnosed through a series of objective tests that our therapists perform. Those tests are purposefully attempting to exacerbate symptoms in order to confirm the diagnosis.
Our clients have concerns that their injury is a rotator cuff tear, but an injury to the rotator cuff muscles or tendons has a very different presentation. Clients with rotator cuff tears present with pain that is worse at night, an inability to lay on that shoulder without pain, and inability to lift the arm overhead due to weakness, and an inability to hold the arm overhead due to pain and/or weakness.
Sometimes shoulder impingement can be confused with the early stages of adhesive capsulitis (also known as frozen shoulder). Frozen shoulder is typically idiopathic in nature, meaning that there is no known cause for why it began. In contrast, there is typically an explanation for why shoulder impingement has occurred (recent changes in activity or exercise regimen, etc.). Frozen shoulder also results in gradually worsening stiffness of the shoulder joint, which is not a finding associated with shoulder impingement.
How to fix shoulder impingement: shoulder impingement treatment
According to this systematic review of randomized controlled trials, shoulder impingement syndrome can be treated successfully through conservative means like physical therapy.
The research is clear that exercise therapy should be the primary treatment intervention to address shoulder impingement. Manual therapy interventions are recommended as well as an adjunct therapy, according to this study.
Treatment for shoulder impingement should address the impairments found on clinical examination. These are the most common impairments for shoulder impingement:
Decreased strength and endurance of the rotator cuff and scapular muscles
Tightness in the posterior shoulder (behind the shoulder)
Decreased shoulder internal rotation range of motion
Shortened pectoralis minor muscle length
Tissue stiffness in the infraspinatus muscle (posterior rotator cuff muscle)
Decreased mobility of the thoracic spine (especially into extension)
Our therapists start by helping you to decrease your pain through activity modifications, education regarding sleeping positions, and isometric exercises. Recent evidence identified 7 key themes for advice and education for those dealing with subacromial pain syndrome: exercise intensity and pain response, activity modification advice, posture advice, pain self-management advice, pathoanatomical and diagnosis information, behavioral approaches, and pain biology advice. Our therapists take great pride in providing you with empowering education to help you take control of your situation.
Manual therapy is helpful in the initial phase of treatment to enhance short-term improvements in pain and function. Manual therapy techniques are beneficial to modulate pain and to complement exercise to improve mobility, muscle activity, and strength. Our therapists utilize manual therapy techniques that target the thoracic spine, shoulder joint (glenohumeral joint), and the shoulder blade (scapulothoracic joint). According to the literature, these are the areas that should be addressed in patients with subacromial pain syndrome.
When symptoms are less irritable, our therapists will transition from exercises with a symptom modulation focus to interventions that target muscle performance and other impairments related to the patient’s movement dysfunction. Exercises to strengthen the posterior rotator cuff and load the shoulder into an elevated position are essential components of an evidence-based program.
Shoulder impingement recovery time: how long does shoulder impingement last?
Shoulder impingement recovery time will be dependent on how long it takes to improve tissue elasticity, capsular mobility, neuromuscular control, and muscular strength. This may vary from case to case, depending on the degree of involvement and the chronicity of the injury. It is reasonable to expect it to take at least 6 weeks, but up to 12 weeks or more to see a resolution of your pain and restoration of your prior level of fitness and function.
Best sleeping position for shoulder impingement
The best sleeping positions for shoulder impingement will be on your back or the non-painful side. Try to avoid sleeping on your stomach or the painful side especially with the arm elevated during the more irritable stages. You can place a pillow under your involved shoulder as you sleep on your uninvolved shoulder. Our therapists find that this can be relieving for some clients.
KT tape for shoulder impingement syndrome
Our physical therapists use KT tape (Kinesiology Tape) as a supplementary treatment for shoulder impingement syndrome. The goal is to utilize KT tape to stimulate the receptors at the skin, therefore facilitating proprioception (awareness) and recruitment of the muscles that stabilize the shoulder blade.
This type of tape is designed to be used temporarily, as the offended tissue heals. Ultimately, we want our clients to rely on their own muscles to do the work.
Shoulder Taping for Shoulder Impingement
Best exercises for shoulder impingement
Side Lying External Rotation
Row with Band
Horizontal Abduction with Elevation - with Band
Quadruped T
Serratus Push Up - Against Wall on Forearms
Shoulder impingement stretches
Foam Roll Thoracic Extension
Pec Doorway Stretch
Overhead Reexposure
Exercises to avoid with shoulder impingement
In the more irritable stages of shoulder impingement, you’ll want to temporarily avoid exercises and activities that involve shoulder elevation overhead, reaching across your body, and reaching behind your back. Examples of these activities include shooting a basketball, throwing and catching a ball, rock climbing, olympic weightlifting, etc.
Vertical Overhead Press - Modification: Horizontal Press
Lat Pull Down / Pull Up - Modification: TRX Lat Row
Lateral Raises - Modification: Scaption Raises
(Partial range of motion as tolerated)
Barbell Back Squat - Modification: Goblet Squat
Closing Remarks
If you are dealing with shoulder impingement syndrome, contact us below to speak with a physical therapist.
Disclaimer: This is not intended to be formal medical advice. Your individual needs should be met by the appropriate health care practitioner. Please consult with a trusted provider.
Dr. Paul Nasri PT, DPT, OCS, COMT
Dr. Vincent Liu PT, DPT
Doctor of Physical Therapy